Hong Kong residents enjoy a sound public healthcare system. However, many aging patients are growing frustrated at waits of up to two years for surgery that is not classified as urgent. Zhou Mo reports from Shenzhen.

Hong Kong’s public health system was ranked as the 14th best globally by Statista’s 2023 Health and Health Systems Index. The World Health Organization (WHO) ranks Hong Kong as the 19th best public healthcare system. There is no crisis in general public healthcare as residents are well provided for.
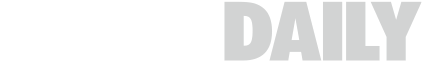
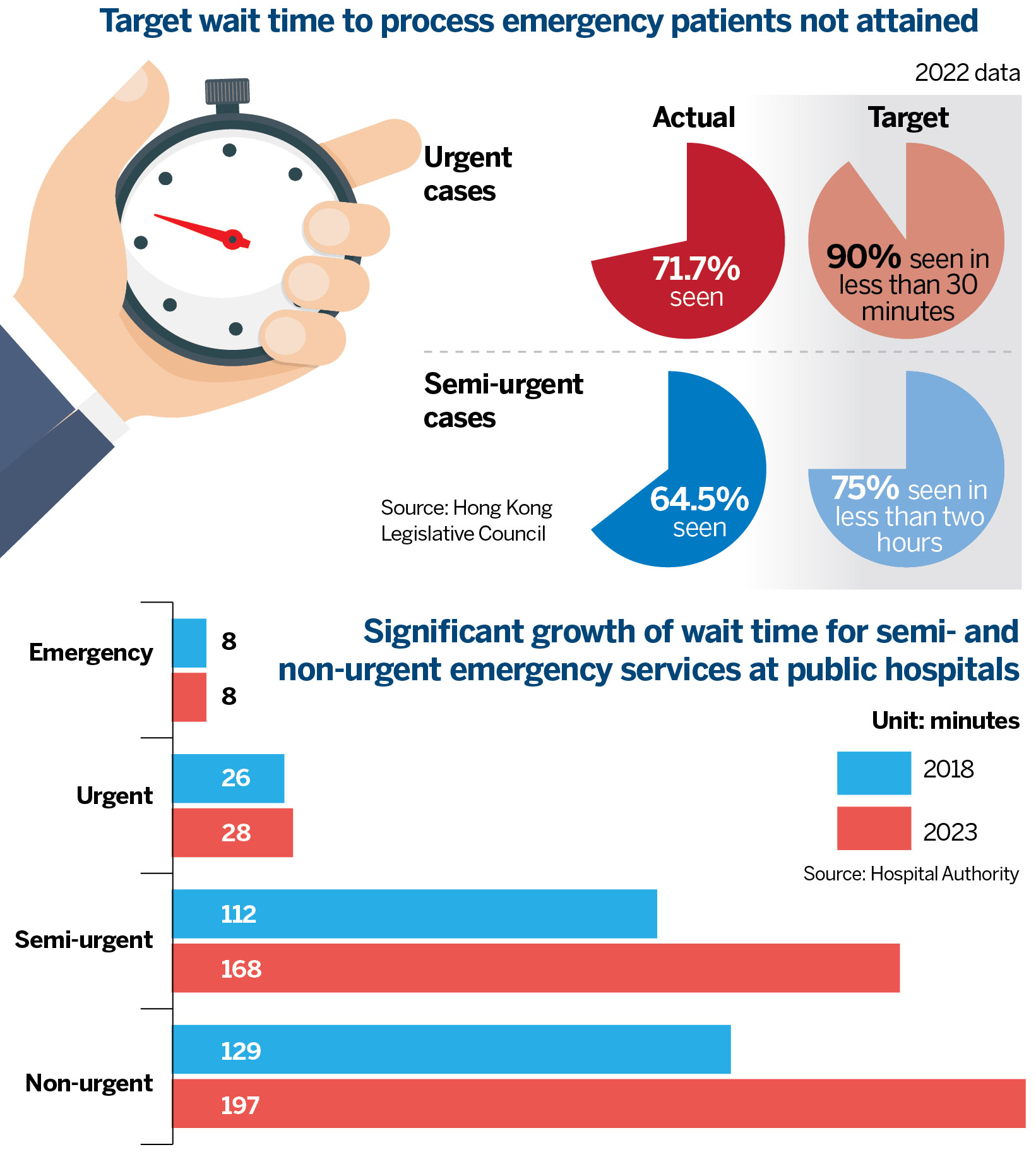
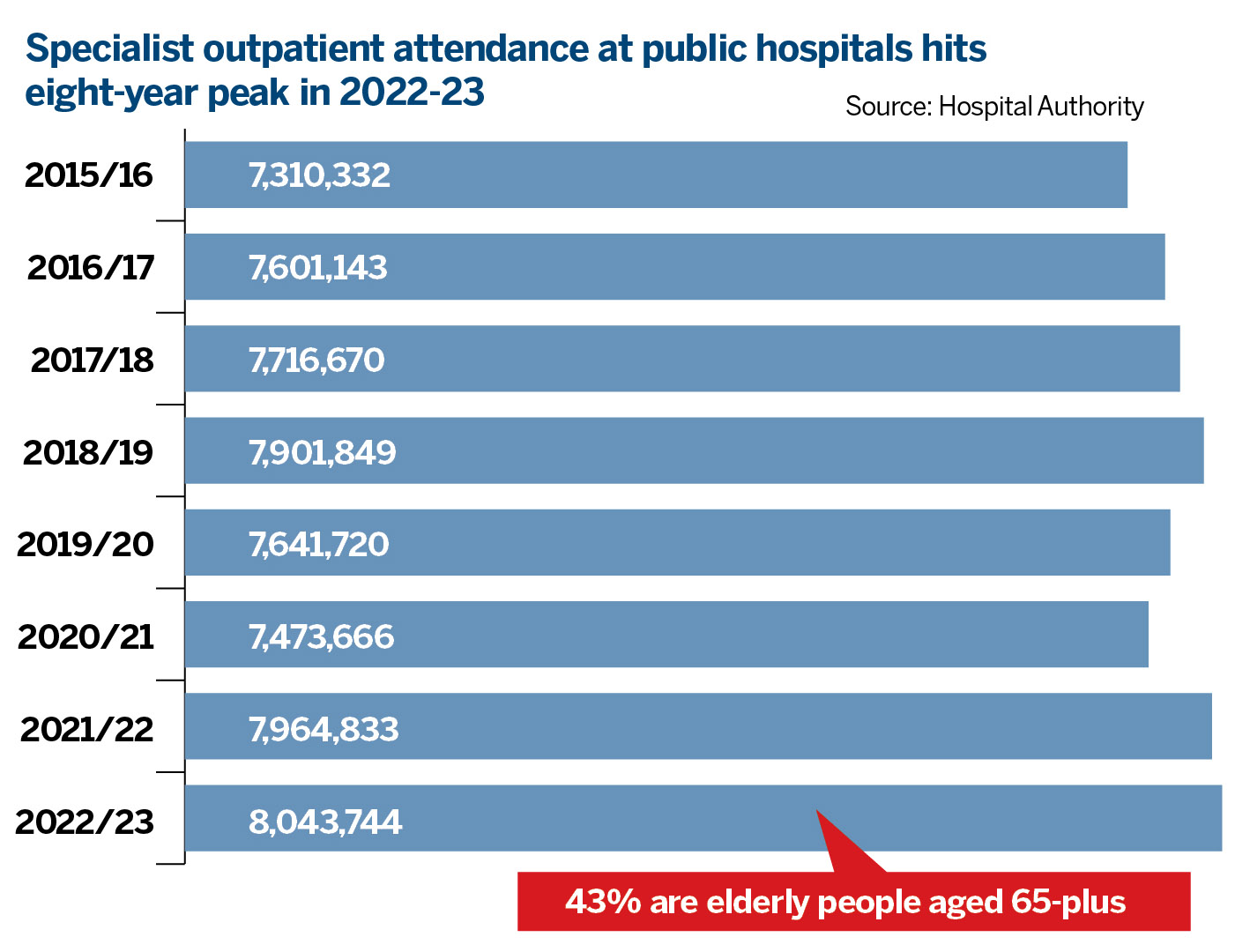
The pain point for elderly residents lies in the long waiting times needed for specialist surgery. The Hospital Authority (HA) classifies new surgery cases into urgent, semi-urgent, and stable. In the 12 months from April 2023 to March 2024, there were 188,330 new cases recorded in Surgery Specialist Outpatient Clinics. These cases comprised 7 percent urgent, 17 percent semi-urgent, and 76 percent stable.
READ MORE: Lo leads delegation in GBA visit to boost medical collaboration
The HA targets to operate urgent cases within two weeks, and semi-urgent cases within 8 weeks. Urgent and semi-urgent cases constitute 24 percent, or 45,097 of the Specialist Surgery Outpatients. How about the 142,609 stable cases needing specialist surgery?
What is most disturbing is the waiting time for specialist surgery of this 76 percent stable category — the median (mid-value) waiting time stretches from 7.5 to 11 months. At the extreme, it can stretch to nearly two years (91 weeks)! This is where the bulk of the frail elderly are suspended.
Every day counts
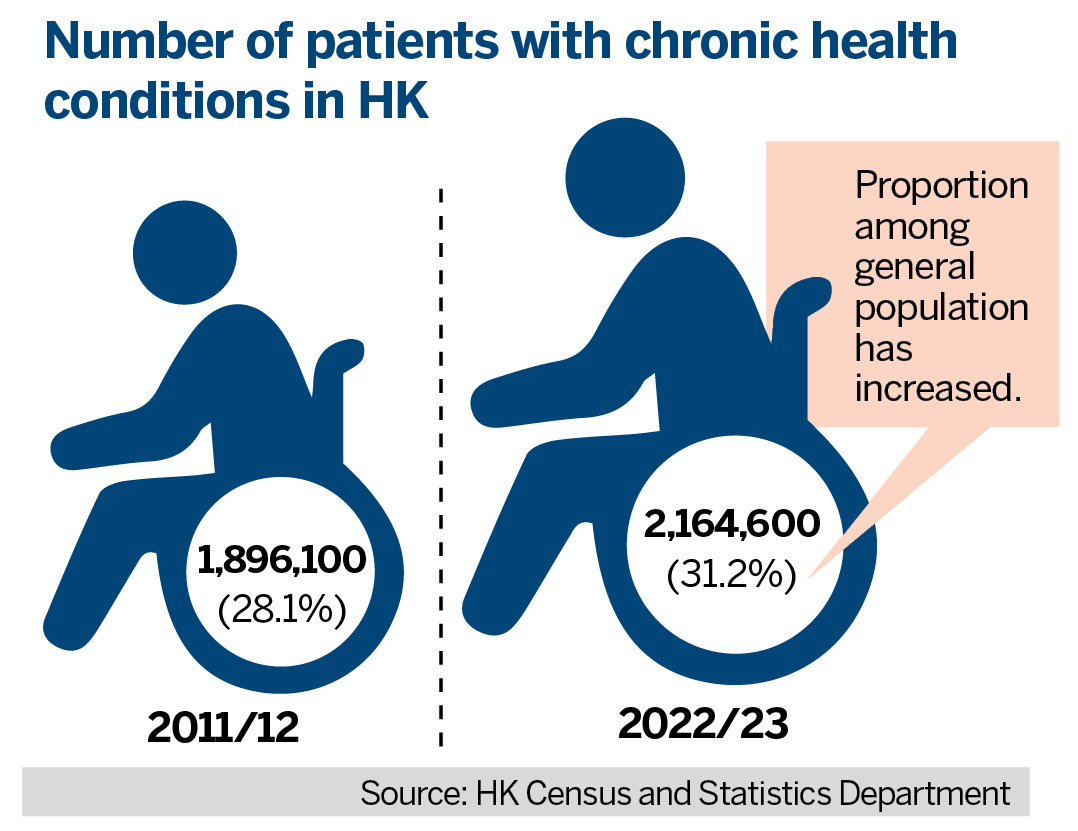
Patients of advanced age, confirmed to need specialist surgery, are anxious to have their medical condition attended to immediately. Few take comfort from being told they are “stable” and therefore can wait another year or two. They count their lives by the day. The longer they remain without the needed surgery, the more their physical condition deteriorates, with mental health suffering further stress.
This pent-up demand has led to a growing exodus of outpatients seeking surgery relief from hospitals across the border in Shenzhen and other cities in the Guangdong-Hong Kong-Macao Greater Bay Area. The Hong Kong Immigration Department recorded more than 53 million cross-border trips last year (not only for medical visits).
According to the government of the Hong Kong Special Administrative Region, the total public and private health expenditures in Hong Kong was around HK$243.2 billion ($31.15 billion) in 2021-22, representing 8.5 percent of GDP.
While the bulk of the city’s working population is gainfully employed, they can afford medical insurance, and get prompt attention in private sector clinics and hospitals. The elderly after retirement, are especially vulnerable.
Some medical institutions operate shuttle buses transporting patients from checkpoints in Hong Kong to the hospitals. Others have tailored online appointment channels for Hong Kong residents. The medical faculties of the University of Hong Kong (HKU) and the Chinese University of Hong Kong (CUHK) have established joint-venture facilities in Shenzhen.
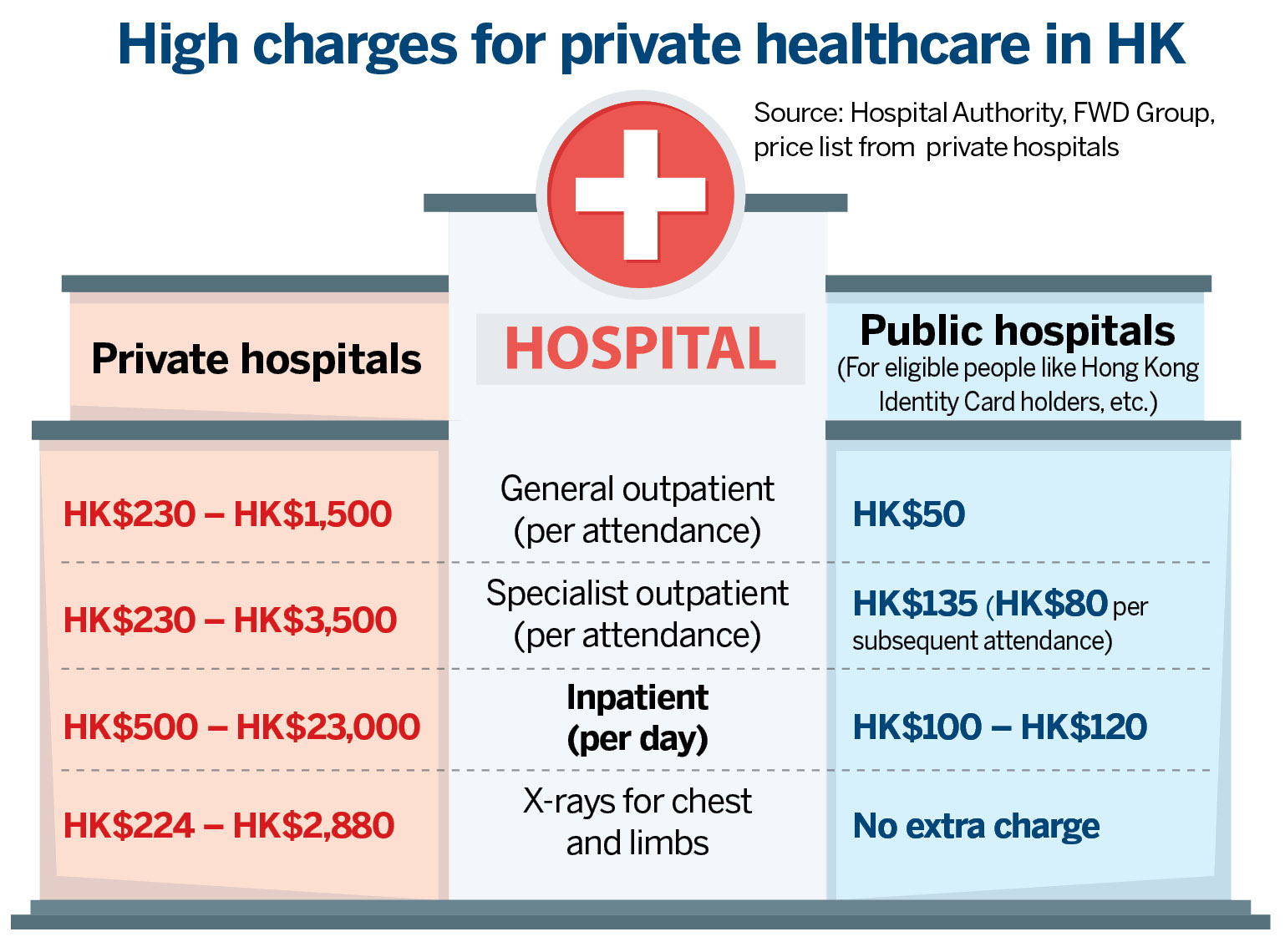
Hong Kong’s public healthcare system is one of the most generous in the world, with the local government bearing roughly 95 percent of inpatient and clinical expenses. According to official statistics, general consultation and specialist consultation fees in public hospitals are HK$50 and HK$80 for non-first-time local patients, respectively. Inpatient service costs HK$100 to HK$120 per day.
By comparison, medical costs in private hospitals are staggeringly expensive. Miss Chan went to a Shenzhen hospital for gastroscopy, which cost her less than 1,000 yuan ($140). The same examination in a Hong Kong private hospital could be 10 times the cost.
Welfare portability
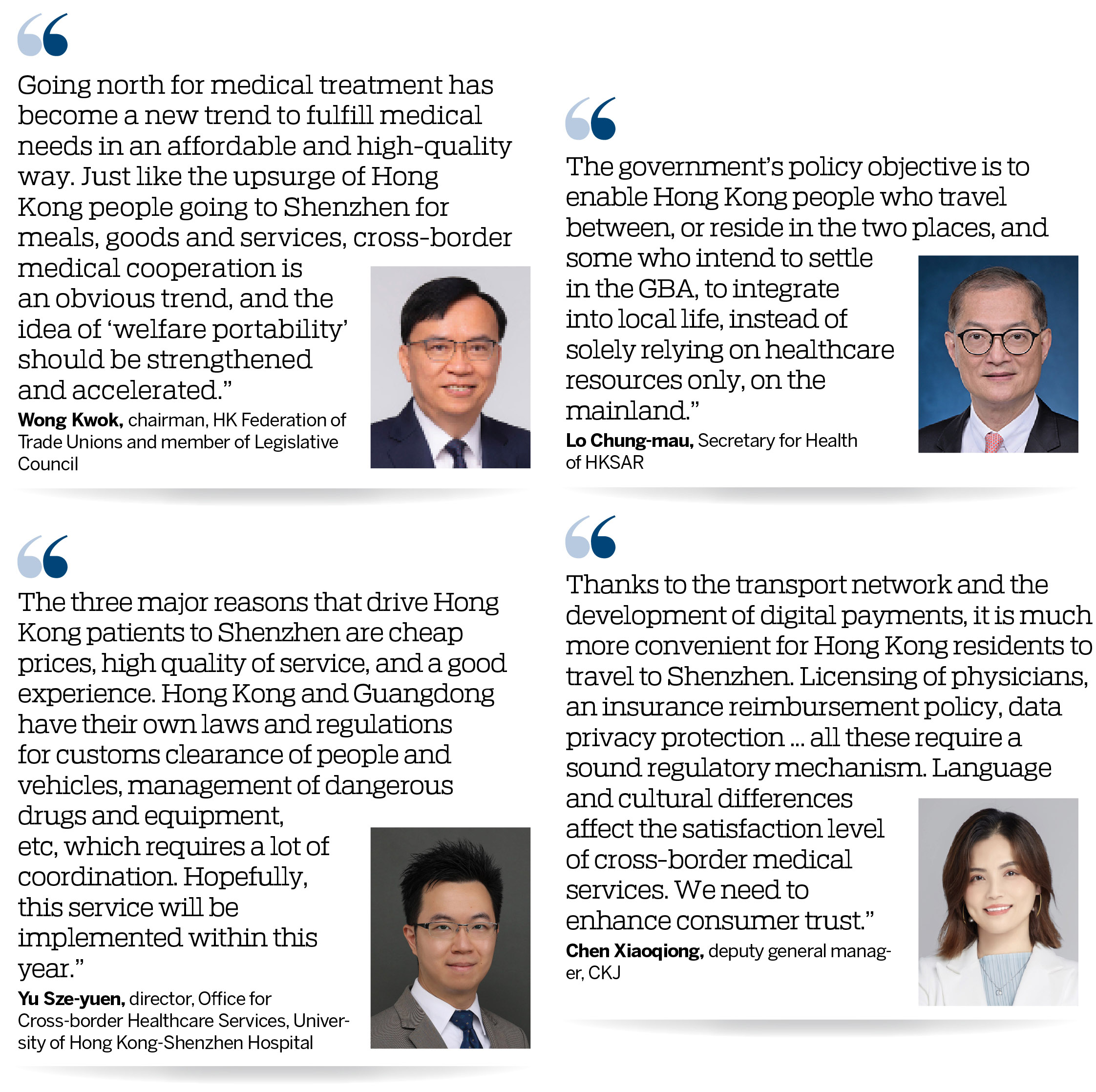
Wong Kwok, chairman of the Hong Kong Federation of Trade Unions and a member of the Legislative Council, says: “Going north for medical treatment has become a new trend to fulfill medical needs in an affordable and high-quality way. Just like the upsurge of Hong Kong people going to Shenzhen for meals, goods and services, cross-border medical cooperation is an obvious trend, and the idea of ‘welfare portability’ should be strengthened and accelerated.”
Yu Sze-yuen, director of the Office for Cross-border Healthcare Services at the University of Hong Kong-Shenzhen Hospital, said the three major reasons that drive Hong Kong patients to Shenzhen are “cheap prices, high quality of service and a good experience”. According to Yu, Hong Kong patients paid 138,000 visits to the hospital between February 2023 and February 2024.
Chen Xiaoqiong, deputy general manager of CKJ, a dental organization in Shenzhen, said: “The consumption patterns of Hong Kong residents have changed a lot since the border reopening. Thanks to improvements in the transport network and the development of digital payments, it has become much easier and more convenient for Hong Kong residents to travel to Shenzhen.”
CKJ has been included in the HKSAR government’s Elderly Health Care Voucher GBA Pilot Scheme. “They have gained more knowledge about the Chinese mainland and the convenience of healthcare there,” added Chen. The organization received over 40,000 visits by Hong Kong patients in the first quarter. “The average monthly number of visits by Hong Kong patients this year stands at 14,000, compared with 10,000 last year,” she said.
To facilitate Hong Kong residents seeking medical services across the border, Hong Kong and Macao Medicine and Equipment Connect was launched, allowing medicine and medical devices that are on the Hong Kong market to be used in designated medical institutions in the Guangdong-Hong Kong-Macao Greater Bay Area after approval. As of mid-January, 28 drugs and 28 medical equipment were approved for use in 19 medical institutions in cities of the GBA.
Elderly voucher program
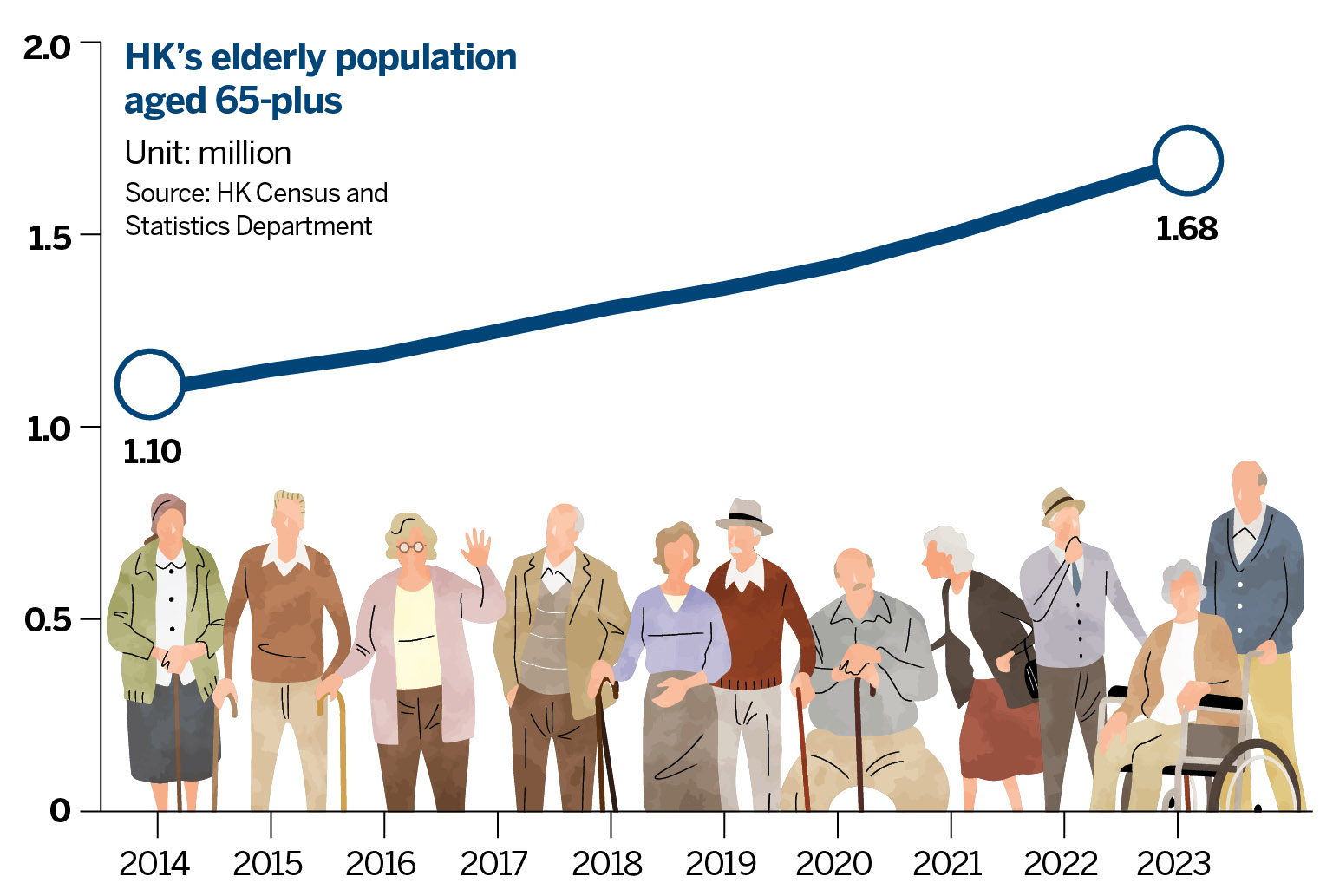
The HKSAR government in February announced the inclusion of seven medical institutions in the GBA in its Elderly Health Care Voucher (EHCV) GBA Pilot Scheme, which ensures about 1.7 million elderly people are eligible to use healthcare vouchers to pay for outpatient healthcare services in four Guangdong cities — Guangzhou, Shenzhen, Dongguan and Zhongshan.
The Health Bureau announced in March that the Pilot Scheme for Supporting Patients of the Hospital Authority in the GBA would be extended until the end of March 2025. Under the program, launched in May 2023, eligible patients pay a consultation fee of 100 yuan at HKU-SZH, while the remaining fee is subsidized by the government, subject to a cap of 2,000 yuan. Over 4,000 patients had enrolled in the program by the end of February.
“Cross-border medical cooperation is only at a preliminary stage, and the overall process has to be accelerated,” said Wong. He noted that the usage of EHCV has room to be expanded further to 3A hospitals or accredited private medical institutions in the GBA cities, as more Hong Kong people choose to settle or retire there.
“The recent announcement of seven more GBA medical institutions to be included in the EHCV GBA Pilot Scheme merely widens the door to ‘welfare portability’. There is still a lot of work to be done in the overall integration of medical systems between the two places.” Comparing Macao with Hong Kong, Wong said Macao’s medical insurance subsidies were extended to nine mainland cities in the GBA in 2022 for residents aged 65 or older, 10 years old or younger, primary and secondary school students, and those with disabilities. “Macao has done it, so can Hong Kong,” said Wong.
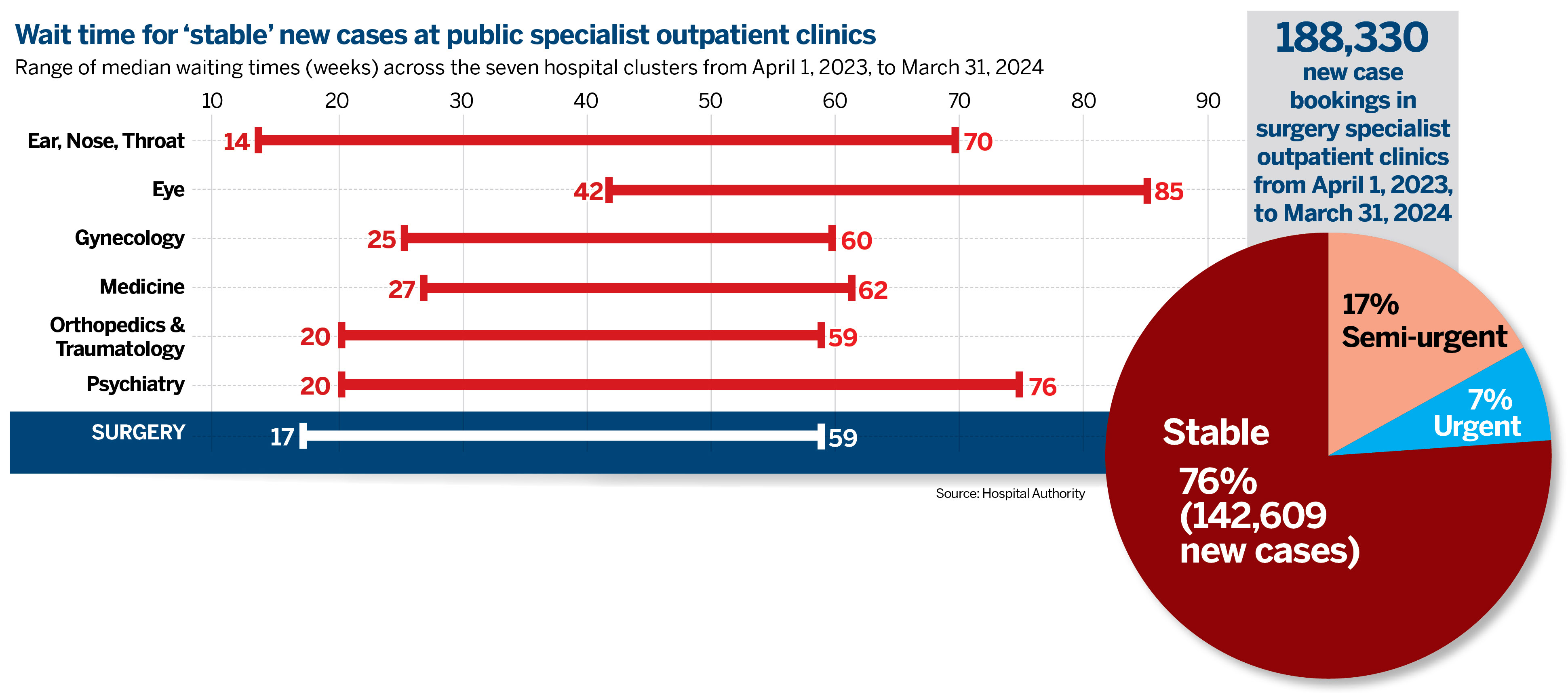
In his 2023 Policy Address, Chief Executive John Lee Ka-chiu stressed the importance of making good use of healthcare services in the GBA. Secretary for Health Lo Chung-mau elaborated, “The government is exploring with suitable GBA healthcare institutions the arrangements to purchase healthcare services. The idea is to start with healthcare services of high demand and lower risks, such as investigation or imaging services, and to devise a service model for the purchase and specific arrangements with compliance of relevant laws and regulations of both places.”
Lo said the government will continue to monitor the progress of cross-border healthcare collaboration initiatives and explore feasible measures to support medical needs of Hong Kong residents more effectively. “The government’s policy objective is to enable Hong Kong people who travel between, or reside in the two places, and some who intend to settle in the GBA, to integrate into local life, instead of solely relying on healthcare resources only, on the mainland.”
Cross-border ambulances
The HKSAR government is also discussing with governments of other cities in the GBA the provision of cross-border ambulance services to enable direct point-to-point hospital transfer of patients, the Policy Address stated.
In the current practice, patients being transferred from a Shenzhen hospital to one in Hong Kong, have to get off the ambulance, clear customs, then get into another vehicle on the other side of the border. That is difficult for those in critical condition. Chen from CKJ says she believes cross-border healthcare is a long-term trend and such demand will grow as regional integration in the GBA deepens.
Yu noted that the provision of cross-border ambulance service involves administrative work across different government departments. “Hong Kong and Guangdong have their own laws and regulations regarding customs clearance of people and vehicles, management of dangerous drugs and equipment, etc, which requires a lot of coordination,” he said. “Hopefully, this service will be implemented within this year.”
Regulatory alignment
Differences in laws and regulations between Hong Kong and the mainland present a major obstacle for medical integration in the meantime. “Licensing of physicians, insurance reimbursement policy, data privacy protection ... all these issues require a sound regulatory mechanism,” Chen noted. Language and cultural differences affect the satisfaction level of patients for cross-border medical services, she added. “We need to enhance consumer trust.”
ALSO READ: HK's eHealth app to facilitate cross-boundary access to electronic medical records
Wong called for comprehensive reform of current licensing examinations, and the launch of new bridging courses, so that experienced doctors from the mainland and abroad can have clear channels to connect and align with Hong Kong professionals.
Meanwhile, “to alleviate a manpower shortage, Hong Kong can establish an ‘associate doctor’ system through limited registration for both overseas medical talent and those who have been practicing as ‘community doctors’ in the city,” he said. “With these pragmatic adjustments, the system can better utilize these professionals and thus effectively protect the rights of patients.”
What's next
1. Align cross-border regulations for medical services access.
2. Accredit mainland and global professionals to work in HK.
3. Implement direct cross-border ambulance services.
4. Integrate the best medical services of HK and GBA mainland cities seamlessly.
Contact the writer at sally@chinadailyhk.com